Distinguish among the different parts (gross and histological) of the alimentary canal in terms of structure and function.................
This picture from the Anatomy and Physiology textbook* explains the basic layers of all portions of the alimentary canal. One of the greatest hurdles to overcome with the alimentary canal is the understanding that while all layers have an internal epithelium for the mucosa, each of those layers will have a different type of epithelium that relates to the structures function. For example the mouth and esophagus have an epithelium layer of stratified squamous to protect them from abrasion. The stomach and the small intestine are both lined with simple columnar epithelium yet the stomach epithelium is designed for secretion of gastric juices while the small intestines epithelium is designed for absorption.
Nurse's Note: Damage to the stomach's epithelial lining can lead to gastric ulcers which can cause severe stomach pain. Once thought to be caused by certain medications and ingesting spicey food, the H.Pylori bacteria is now thought to be the most common cause.
Page List
▼
Saturday, April 23, 2011
Objective 57: Lacteals
Justify the role of lacteals in transporting products of digestion..............
A lacteal is a lymphatic capillary that absorbs dietary fats in the villi of the small intestine. http://en.wikipedia.org/wiki/Lacteal
A lacteal is a lymphatic capillary that absorbs dietary fats in the villi of the small intestine. http://en.wikipedia.org/wiki/Lacteal
 |
| http://en.wikipedia.org/wiki/Lacteal I'm really not sure how to reflect on this except to say that it seems pretty basic. The villi in the small intestine contain both a lacteal or lymph capillary and a capilary bed. The digested food is absorbed into the epithelium and sent throughout the body via the lymph capillary and the capillary bed. Also, this lacteal picture reminds me of a sunflower ! |
Objective 59: Microscopic Anatomy of the Liver
Appreciate the microscopic anatomy of the liver.....
 |
| Liver |
 |
Understanding that the livers overall function in the body is to filter and process the blood supply helps with understanding the microscopic anatomy. The photo that I took in lab helps me in grasping the concept that the liver lobules are a six-sided shape with a central vein running through it. The picture from the Anatomy and Physiology text* shows in depth what occurs at the portal triad on each one of those corners. Reading through the text explained the many facets of the liver including:
Glycogen storage
Decomposition of RBC'S
Plasma protein synthesis
Hormone production and detoxification
Bile production
Nurse's Note: Two common diagnoses that pertain to the liver are Hepatitis, a long-term, chromic and potentially fatal infection of the liver caused by a virus and Cirrhosis, a chronic infection of the liver caused by alcoholism.
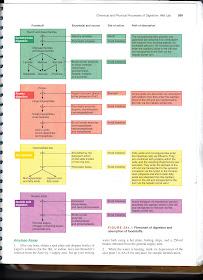
Objective 58: Hormones and Digestion
Relay structure and function of the endocrine system to digestion...........
These two pictures from the Anatomy and Physiology textbook* along with time in both lab discovery and lecture gave a full understanding of the role that the endocrine system plays in digestion. The pancreas is labeled as both and endocrine and exocrine gland. Its exocrine functions include the release of enzymes that aid in digestion and its endocrine functions include the release of both insulin by the beta cells and glucacon by the alpha cells. These two secretions work antagonistically to one another to maintain the proper amount of glucose in both the blood and the cells.
I had an "AHA" moment while listening to one of the podcasts regarding glucagon and insulin. It was so "AHA" and had me so turned around that I actually had to get Jeremy to explain it to me again! While listening to the podcasts on the endocrine system the question was posed "What would be the result of too much insulin in the blood stream"? I know the answer to this, I thought! High blood sugar! WRONG, so WRONG! The answer was hypoglycemia. What? How can that be? I was so perplexed that I actually had to grab Jeremy in the parking lot at school, make him listen to that section of the podcast and then pretty much force him to repeatedly explain it to me. He laughed as he explained that I apparently had the functions of insulin and glucagon backwards. Insulin actually moves the glucose into the cell while glucagon breaks down glycogen from the liver and puts glucose back into the blood stream.
Thank you, Jeremy for setting me straight!
Nurse's Note: Diabetes Mellitus occurs when there is too little insulin in the blood and glucose can not be effectively moved into the cells. There are three cardinal signs of Diabetes Mellitus. These include polyuria or excessive urine output, polydipsia or excessive thirst, and polyphagia or excessive hunger.
Objectives 60 & 61: Chemical forms that major food classes are absorbed and pancreatic juices
State the chemical forms in which the major food classes are absorbed and describing enzymatic and bicarbonate content of pancreatic juices.
This sheet from the Anatomy and Physiology Laboratory Manual** gave a thorough description of how the major food classes were broken down into chemical forms for absorption. In addition to the chart shown here, lab exercises were done to increase understanding of how the foods were broken down and what organs played a mjor part in making that happen. In addition, the chart also highlights the pancreatic enzymes that play a part in digestion of these food sources such as pancreatic amylase that works to breakdown carbohydrates, Trypsin that works to break down proteins, pancreatic lipase that works on fats, and pancreatic ribonuclease and deoxyribnuclease that breakdown amino acids. All of these enzymes are secreted from the pancreas in an inactive form and are activated in the small intestine.
Nurse's Note: Carbohydrates, proteins, and fats are considered macronutrients because our body requries these food sources in large amounts in order to function properly. Carbohydrates are the body's major source of energy and the only source that the central nervous system can use. Proteins fuel and build muscle while fat offers additional energy and protection of the organs.
Objectives 63 & 66: Renal corpuslces and tubules and tasks of the nephrons
Describing the structure and function of the renal corpuscles and tubules and identifying the three basic tasks performed by the nephrons and tubules.....
 |
| Picture from Anatomy and Physiology textbook* |
I have to say, I've really enjoyed this textbook. Its been really easy to read and follow along with compared to some of the science texts that I've used in other classes. The fact that the text and picture are both color coordinated to show the three processes that the nephrons perform and where it occurs in the renal corpuscle and tubules was a geat starting place in understanding these objectives. Breaking the processes down like this makes them seem less overwhelming.
Objectives 52, 65, & 69: Blood pressure and volume, juxtoglomerular cells and renin, and water excess and dehydration
Detailing the kidneys involvement in blood pressure and volume regulation, stating the importance of the juxtoglomerular cells in secretion of renin, and assessing how water excess and dehydration affect kidney function.....
Understanding how the kidneys work to maintain blood volume and blood pressure is tricky because there are multiple methods (and hormones) that can be involved in doing this. I had a good understanding of the hormones that were involved including aldosterone and ADH, but was a little bit iffy on where renin fit into the process. Watching this video where they gave a step by step explanation of how the release of each hormone causes a cascade effect onto another organ helped me to get a better grasp of the entire process.
In all of the processes listed above there is one additional factor that plays a large part in maintaining body homeostasis and that is WATER! So its important to discuss and understand how water excess or dehydration ties into maintaining blood volume and blood pressure as well. When the body becomes dehydrated due to excessive fluid loss or a decrease in fluid intake the extracellular fluid becomes a hypertonic solution for the cells. This means that the water in the cells will move out into the extracellular fluid (following those salts or solutes like water always does!) causing the cell to crenate. On the other hand, when we have excessive amounts of fluid in the system, the cells are in a hypotonic solution. So the water in the extracellular fluid will move into the cells causing them to overfill and lyse.
Nurse's Note: Diuretics are commonly prescribed along with antihypertensive medications to treat high blood pressure. Just another example of how blood pressure and blood volume tie in together.
Objective 69: Volume and Electrolyte Content
Contrast volume and electrolyte content in inter and extracellular fluid compartments....
Looking at the first chart shown gives a very specific breakdown of the total body water and how it is broken down into the body's "fluid compartments". The second chart gave an understanding of where the electrolytes are carried in the body's fluids. The second chart showed results that I actually expected based on previous knowledge regarding depolarization events that take place in the nervous and muscular systems. We were taught that there is a higher volume of potassium inside the cells and a higher volume of sodium on the outside of the cells. The influx of sodium ions is what causes the cell to depolarize so that the signal can be transmitted.
Nurse's Note: Many processes in the body, especially in the brain, nervous system, and muscles, require electrical signals for communication. The movement of sodium is critical in generation of these electrical signals. Too much or too little sodium therefore can cause cells to malfunction, and extremes in the blood sodium levels can be fatal.
 |
| Major fluid compartments of the body from Anatomy and Physiology textbook p.868* |
 |
| Electrolyte composition of body fluids from Anatomy and Physiology textbook p. 869* |
Nurse's Note: Many processes in the body, especially in the brain, nervous system, and muscles, require electrical signals for communication. The movement of sodium is critical in generation of these electrical signals. Too much or too little sodium therefore can cause cells to malfunction, and extremes in the blood sodium levels can be fatal.
- Increased sodium (hypernatremia) in the blood occurs whenever there is excess sodium in relation to water. There are numerous causes of hypernatremia; these may include kidney disease, too little water intake, and loss of water due to diarrhea and/or vomiting.
- A decreased concentration of sodium (hyponatremia) occurs whenever there is a relative increase in the amount of body water relative to sodium. This happens with some diseases of the liver and kidney, in patients with congestive heart failure, in burn victims, and in numerous other conditions.
Monday, April 18, 2011
Objectives 51, 55, & 62. Kidney function, Path of blood, and Renal anatomy
Describing kidney function, tracing the path of blood flow through the kidneys and describing internal and external gross renal anatomy.......
So, as you know, we weren't able to do our in-class lecture on the urinary system, and we had to do an online lecture for this portion of the text. Well, I have to say that I'm really glad that I didn't take this class online. I enjoy the online lectures, but they always leave me feeling like I've missed ALOT! (I think I actually told you this when I came into the class a week late and had to do the endocrine lectures online!) Anyway, so I went to YouTube looking for videos to help me get a better grasp on the urinary system and this is what I came across. I think that it really helped! Watching this video from the Greater Pacific Company helped me to get a visual understanding of how the kidneys function including understanding how they receive blood from the arterioles and send it into the Bowmans capsule portion of the nephrons for filtering in the Glomerulus, a mass of intertwined capillaries. In the Glomerulus there's a bit of a slow down that allows substances to be filtered due to the fact that the arteriole ENTERING is larger than the arteriole EXITING (I sort of think of a lymph node here where the fact that there are more afferent vessels than efferent vessels gives the lymph fluid time to be filtered).
Nurse's Note: Diabetes Mellitus and Hypertension are the most common causes of End Stage Renal Disease, where the kidneys stop forming filtrate and metabolic wastes build up in the blood stream. The most common treatment for this is hemodialysis where the patient is hooked up to a machine that actually pulls the blood from their bodies in order to filter the wastes from it before the blood is returned into the body. Fluid and Electrolyte testing is done on the patient prior to dialysis being performed so that any electrolytes that are missing or lacking from the blood can be added into the filtered blood as it is returned to the body. Often in a patient that requires frequent dialysis, a fistula is done. A fistula is the connection of an artery and a vein inside the body to provide a permanent port for dialysis. This port helps to strengthen the blood vessel so that insertion of needles for dialysis treatments are easier. Fistula's are commonly tested for Thrill ,a constant palpable vibration at the fistula site, and Bruit, a soft, low-pitched noise heard through the stethoscope when placed on the fistula to ensure that the blood is still flowing properly through the fistula.
Objective 64: Transport of Carbon Dioxide and Oxygen
Discuss how oxygen and carbon dioxide are transported......
Oxygen transport
About 98.5% of the oxygen in a sample of arterial blood in a healthy human breathing air at sea-level pressure is chemically combined with the Hgb. About 1.5% is physically dissolved in the other blood liquids and not connected to Hgb. The hemoglobin molecule is the primary transporter of oxygen in mammals and many other species (for exceptions, see below). Hemoglobin has an oxygen binding capacity of between 1.36 and 1.37 ml O2 per gram Hemoglobin, which increases the total blood oxygen capacity seventyfold, compared to if oxygen solely was carried by its solubility of 0.03 mL O2 per liter blood per mmHg partial pressure of oxygen (approximately 100 mmHg in arteries). With the exception of pulmonary and umbilical arteries and their corresponding veins, arteries carry oxygenated blood away from the heart and deliver it to the body via arterioles and capillaries, where the oxygen is consumed; afterwards, venules, and veins carry deoxygenated blood back to the heart. Under normal conditions in adult humans at rest; hemoglobin in blood leaving the lungs is about 98–99% saturated with oxygen, achieving an oxygen delivery of between 950 - 1150 mL/min to the body. In a healthy adult at rest, oxygen consumption is approximately 200 - 250 mL/min, and deoxygenated blood returning to the lungs is still approximately 75% (70 to 78%) saturated. Increased oxygen consumption during sustained exercise reduces the oxygen saturation of venous blood, which can reach less than 15% in a trained athlete; although breathing rate and blood flow increase to compensate, oxygen saturation in arterial blood can drop to 95% or less under these conditions. Oxygen saturation this low is considered dangerous in an individual at rest (for instance, during surgery under anesthesia. Sustained hypoxia (oxygenation of less than 90%), is dangerous to health, and severe hypoxia (saturations of less than 30%) may be rapidly fatal. A fetus, receiving oxygen via the placenta, is exposed to much lower oxygen pressures (about 21% of the level found in an adult's lungs), and, so, fetuses produce another form of hemoglobin with a much higher affinity for oxygen (hemoglobin F) in order to function under these conditions.
Carbon dioxide transport:
When blood flows through capillaries, carbon dioxide diffuses from the tissues into the blood. Some carbon dioxide is dissolved in the blood. A part of CO2 reacts with hemoglobin and other proteins to form carbamino compounds. The remaining carbon dioxide is converted to bicarbonate and hydrogen ions through the action of RBC carbonic anhydrase. Most carbon dioxide is transported through the blood in the form of bicarbonate ions. Carbon dioxide (CO2), the main cellular waste product is carried in blood mainly dissolved in plasma, in equilibrium with bicarbonate (HCO3-) and carbonic acid (H2CO3). 86–90% of CO2 in the body is converted into carbonic acid, which can quickly turn into bicarbonate, the chemical equilibrium being important in the pH buffering of plasma. Blood pH is kept in a narrow range (pH between 7.35 and 7.45).
Transport of hydrogen ions:
Some oxyhemoglobin loses oxygen and becomes deoxyhemoglobin. Deoxyhemoglobin binds most of the hydrogen ions as it has a much greater affinity for more hydrogen than does oxyhemoglobin.
http://en.wikipedia.org/wiki/Blood
Ok, so there's alot of information covered above! We've been buzzing around this subject since back in BIO-100 when we talked about carrier proteins and Mrs. Gess did the football player tucking the ball into a safe hold in order to get it up the field. In this case, the football player is hemoglobin and oxygen is the ball. The only difference is that hemoglobin is like a multi-handed player because it can actually carry up to four oxygen's at a time!
We touched further on this subject when we were discussing the physical components of blood and the fact that respiratory gases are included in those physical components, and that they also play a part in the overall pH of the blood. Over seventy percent of the carbon dioxide in the blood travels as bicabonate ion and is quickly transported to the lungs.
Nurse's Note: Oxygen saturation, also known as your O2 sat, is considered one of your basic vital signs in a hospital setting. Your O2 sat is measured by the use of a handheld machine called a pulse-oximeter. This device clips onto either a finger, toe, or earlobe and determines the amount of oxygen available to your tissues in just a few seconds. Nail polish should be removed prior to taking the reading if a fingertip is the desired testing site as it can misconstrue the reading. An O2 sat below 95% is considered an emergency or crisis situation that requires immediate attention and is often referred to as Hypoxia.
Objective 56, 68 & 70: Acidosis and Alkalosis
Examining differences in metabolic and respiratory acidosis and alkalosis, recognizing how chemical buffers interact to protect the body against lethal changes in pH, and recognizing how the lungs and kidneys interact to protect the body agains lethal changes in pH.
Reading through this chart and sections of the Anatomy and Physiology text book* helped me to understand that the terms respiratory acidosis and alkalosis are strictly related to respiratory function and are reflective of the amount of carbon dioxide in the blood. Metabolic acidosis and alkalosis are reflective of other acid-base balances in the blood, and present with an effect on the GI tract.
The chemical buffer systems that affect the body's pH were relatively familiar territory based on previous lectures over the last three semester. Understanding that hydrogen ion is the predominant ion that makes the blood more acidic comes from a Bio-100 lecture concerning the acid-base system. We looked further into the hydrogen ion in this class in discussing how carbon dioxide is carried in the blood. In Bio-100 we also discussed the process of glycolysis, where glucose products were broken down in an anaerobic environment that caused the release of lactic acid. The key point here is that for every action in the body, there is also a reaction. That is where the chemical buffering systems like the bicarbonate buffer system, the phosphate buffer system and the protein buffer system come into play. Any time one of the above actions occur releasing acids into the blood, one of the chemical buffering systems reacts to maintain the narrow range of pH required for homeostasis.
Understanding that the kidneys and lungs are the two most vital organs in managing the body's changes in pH comes from an understanding of how these organs work and what they're "job" in the body is. The lungs help to maintain the body's pH by expelling carbon dioxide through respiration while the kidneys excrete other acids that are a by-product of cellular metabolism such as lactic and uric acids.
Reading through this chart and sections of the Anatomy and Physiology text book* helped me to understand that the terms respiratory acidosis and alkalosis are strictly related to respiratory function and are reflective of the amount of carbon dioxide in the blood. Metabolic acidosis and alkalosis are reflective of other acid-base balances in the blood, and present with an effect on the GI tract.
The chemical buffer systems that affect the body's pH were relatively familiar territory based on previous lectures over the last three semester. Understanding that hydrogen ion is the predominant ion that makes the blood more acidic comes from a Bio-100 lecture concerning the acid-base system. We looked further into the hydrogen ion in this class in discussing how carbon dioxide is carried in the blood. In Bio-100 we also discussed the process of glycolysis, where glucose products were broken down in an anaerobic environment that caused the release of lactic acid. The key point here is that for every action in the body, there is also a reaction. That is where the chemical buffering systems like the bicarbonate buffer system, the phosphate buffer system and the protein buffer system come into play. Any time one of the above actions occur releasing acids into the blood, one of the chemical buffering systems reacts to maintain the narrow range of pH required for homeostasis.
Understanding that the kidneys and lungs are the two most vital organs in managing the body's changes in pH comes from an understanding of how these organs work and what they're "job" in the body is. The lungs help to maintain the body's pH by expelling carbon dioxide through respiration while the kidneys excrete other acids that are a by-product of cellular metabolism such as lactic and uric acids.
Sunday, April 17, 2011
Objective 53: Dalton's Law and Boyle's Law
Define Dalton's law of partial pressure and Boyle's gas law and relate both to respiratory physiology...
In chemistry and physics, Dalton's law (also called Dalton's law of partial pressures) states that the total pressure exerted by a gaseous mixture is equal to the sum of the partial pressures of each individual component in a gas mixture. This empirical law was observed by John Dalton in 1801 and is related to the ideal gas laws. http://en.wikipedia.org/wiki/Dalton%27s_law
Boyle's law (sometimes referred to as the Boyle-Mariotte law) is one of many gas laws and a special case of the ideal gas law. Boyle's law describes the inversely proportional relationship between the absolute pressure and volume of a gas, if the temperature is kept constant within a closed system.[1][2] The law was named after chemist and physicist Robert Boyle, who published the original law in 1662.[3] The law itself can be stated as follows: For a fixed amount of an ideal gas kept at a fixed temperature, P [pressure] and V [volume] are inversely proportional (while one doubles, the other halves). http://en.wikipedia.org/wiki/Boyles_law
Well, lets see here. My initial reaction is HUH? But lets start small. I understand that Boyle's Law directly relates to inspiration and expiration in that these two processes are stimulated by differences in atmospheric pressure and internal pressures. Based on Boyle's Law the internal pressure inside the intrapulmonary space changes based on whether the lungs are expanded or recoiled because the size of the container affects the pressure of the gas that it contains. Especially in a container that change size 12 to 20 times a minute.
Objective 50: Incentive Spirometer Use
Demonstrate spirometer use and examine spirogram data........
The use of incentive spirometers is a task that we covered early on in our nursing labs. The incentive spirometer helps to increase lung volume and prevent atelactasis (or collapsing of the alveoli) in patients who have respiratory issues or are bed-bound following surgery.
Nurse's Note: Encouraging the use of an incentive spirometer is an independent nursing intervention that does not require an order from a physician.
The use of incentive spirometers is a task that we covered early on in our nursing labs. The incentive spirometer helps to increase lung volume and prevent atelactasis (or collapsing of the alveoli) in patients who have respiratory issues or are bed-bound following surgery.
Nurse's Note: Encouraging the use of an incentive spirometer is an independent nursing intervention that does not require an order from a physician.
Objective 45: The neuronal network that controls respiration
Characterize the neuronal network that controls respiration........
This picture provided on P. 731 of the Anatomy & Physiology textbook* helped me to understand that the neuronal network that controls breathing stems from the Pons and the Medulla of the brain. It gives a brief description of the three different respiratory centers; The Pontine that works to smooth breathing patterns, The Ventral that controls the rhythm of respiration, and the Dorsal that receives sensory input.
Nurse's Note: There are terms that are commonly used in the medical field to describe an indiviuals breathing pattern.
These include:
These include:
Eupnea: a normal breathing rate between 12 and 20 breaths per minute.
Dyspnea: Difficulty or pain during breathing.
Apnea: The absence of breathing.
Objectives 46 & 47: Cellular Respiration and Arterial Carbon Dioxide Levels
Relating breathing to cellular respiration and determining how arterial carbon dioxide levels affect ventilation.......
WE DON’T BREATHE BECAUSE OUR LUNGS NEED AIR……. WHAT IS SHE TALKING ABOUT?!
NOW THIS ONE REALLY THREW ME FOR A LOOP!
This statement goes way back to BIO-100. I literally remember my instructor making this comment and thinking, man is she nuts or what?! But WOW, she’s right! Bits and pieces of information over the past three semesters have led to an actual understanding of this statement. So why do we breathe? In Bio-100 we learned (ad-nauseam) about cellular respiration and how the body’s requirements for oxygen actually stem from the mitochondria of the cells needing oxygen in order to break down glucose and other nutrients in order to produce ATP. BUT WAIT, .. THERE’S MORE. This whole process then puts off carbon dioxide as a by-product. Problem is; when carbon dioxide mixes with water it releases hydrogen ions and this in turn makes the blood more acidic. ALMOST THERE!!!! So that acidity is what stimulates the chemoreceptors in the body to say WOAH, TOO MUCH carbon dioxide…BLOW IT OUT! And we do, therefore changing the difference in the atmospheric pressure and the interpulmonary pressure which then causes us to inhale…oxygen, sweet oxygen!~
Nurse's Note: COPD patients will typically have an oxygen saturation rate below what is considered an aceptable rate. The normal mechanism for breathing is when the medulla senses an increase in carbon dioxide and stimulates breathing to increase the rate and depth of respirations. Yet in COPD patients the stimulus to breathe is the decreasing arterial oxygen levels sensed by the peripheral chemoreceptors in the carotid sinus and aortic arch. Therefore, if you give a COPD patient too much oxygen you could essentially oversaturate their body with oxygen and make them lose their drive to breathe.
Nurse's Note: COPD patients will typically have an oxygen saturation rate below what is considered an aceptable rate. The normal mechanism for breathing is when the medulla senses an increase in carbon dioxide and stimulates breathing to increase the rate and depth of respirations. Yet in COPD patients the stimulus to breathe is the decreasing arterial oxygen levels sensed by the peripheral chemoreceptors in the carotid sinus and aortic arch. Therefore, if you give a COPD patient too much oxygen you could essentially oversaturate their body with oxygen and make them lose their drive to breathe.
Objectives 48 & 49: Inhalation and Exhalation/ Inspiration and Exhalation
Delineating the role of muscles and lung elasticity in inhalation and exhalation and Contrasting inspiration and Expiration................
This picture from p. 717 of the Anatomy & Physiology textbook* gives a great overview of the processes that take place during inspiration and expiration. Describing in detail the muscles that are involved in inspiration such as the diaphragm and the external intercostals and then describing how expiration is a passive process that occurs through the recoiling of the elastic lungs. It demonstrates the changes in intrapulmonary pressure that occur in order to stimulate these two processes. I specifically remember having this conversation in class where we talked about the atmospheric pressure that would essentially weigh down on the body causing us to inhale in order to equalize the pressure gradients.
Objective 43 and 44: Respiration
Anatomy, function and histology of the respiratory organs
Understanding the anatomy, function, and histology of the respiratory organs was achieved through multiple avenues. Discussion time in lecture gave an in-depth understanding of the function of the respiratory organs while time spent on dissection and using the microscope in the laboratory helped with understanding the anatomy and histology.
Nurse's Note: Smoking has many negative effects on the respiratory organs including destruction of the protective cilia that line some of these organs. Destruction of these cilia can lead to an increase in pathogens entering the respiratory system and can result in inflammation and infection.